Medicaid
Medicaid is a public health insurance initiative that provides free or low-cost health coverage to individuals with limited income. Individuals and families retain access to essential medical care through participating health providers while avoiding financial hardship that can come from paying for health needs out of pocket. Medicaid is both federal and state funded, though each state manages its own program, resulting in a unique range of benefits and eligibility depending on where an individual lives.
Expanded Medicaid coverage is a provision of the Affordable Care Act (ACA) that makes Medicaid available to nearly all low-income adults, regardless of whether they have dependent children or a disability, up to 138% of the federal poverty level. This expansion, which is optional for states, was designed to cover a “coverage gap” of low-income adults who did not qualify for traditional Medicaid and could not afford private insurance. As of April 2025, 41 states and Washington, D.C. have adopted this expansion.
75.8 million people enrolled in Medicaid1
Reference: 1. Medicaid.gov. March 2025 Medicaid and CHIP Enrollment Data Highlights.
https://www.medicaid.gov/medicaid/program-information/medicaid-and-chip-enrollment-data/report-highlights
Medicaid Eligibility Requirements
Medicaid eligibility is based on a combination of factors: income, household size, age, disability status, and sometimes, immigration status. Thanks to the Affordable Care Act (ACA), those in low-income households, including children, seniors, and adults under age 65 meeting income guidelines, may qualify.
What Medicaid Covers
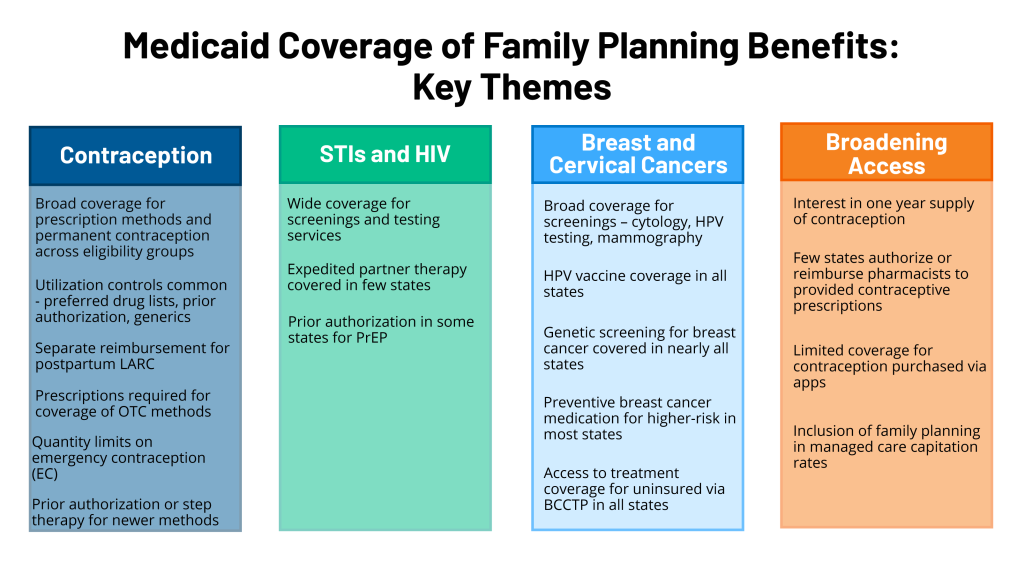
To ensure no health need goes unmet, Medicaid plans carry a set of mandatory benefits set by federal law, including:
- Inpatient and outpatient hospital services
- Early and periodic screening, diagnostic, and treatment services (EPSDT)
- Home health and nursing facility services
- Physician and rural health clinic services
- Laboratory and X-ray services
- Pediatric, family planning, birthing center, and nurse midwife services
- Transportation to medical care
- Inpatient and outpatient psychiatric, behavioral, and mental health services
Each state makes its own decisions about Medicaid expanded coverage, and benefits may include:
- Prescription drugs
- Physical, speech, and occupational therapy
- Other diagnostic and preventive services
- Specialized care, such as dental, vision, and podiatry
Individuals should speak with their state Medicaid office or a certified navigator to fully understand available plan benefits in their area.
How to Apply for Medicaid
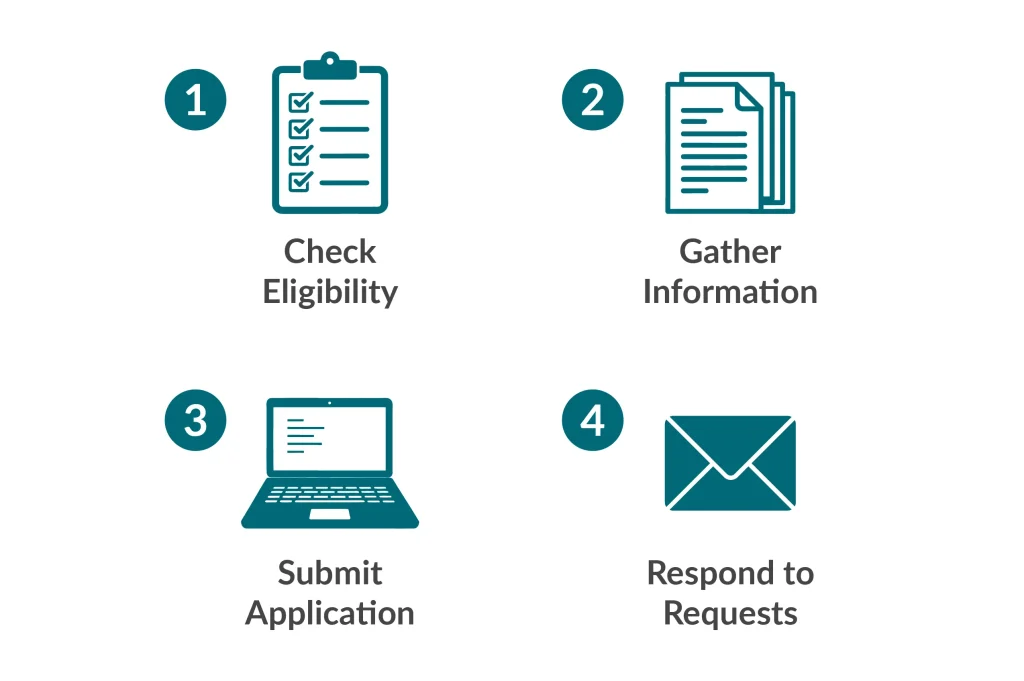
Applications can be submitted in person or online to the local Medicaid office or Health Insurance Marketplace. The Marketplace will forward eligible applicants to the appropriate state agency to secure Medicaid coverage. Individuals need to provide specific documentation, often including:
- Proof of identity
- Social security number
- Proof of monthly cost of living (rent, mortgage, utilities)
- Proof of citizenship or immigration status
- Proof of current income and employment status, such as paystubs and W-2s
- Information on current government benefits received and current insurance plans carried
Approval timelines vary from state to state, but most agencies work to process applications quickly. Individuals often receive a decision within a few weeks. Urgent cases such as pregnancy or medical emergencies may result in temporary or “presumptive” coverage while high-need individuals’ applications are reviewed.
Using Medicaid Once Approved
Approved individuals will receive a notice from their state Medicaid office and an enrollment card to share with healthcare providers and pharmacists. They can first consult the Medicaid network to confirm current providers participate in the program. If they do not, the state Medicaid agency provides resources online for individuals and families to explore the vast network of coverage. Healthcare providers can confirm coverage as well when presented with a Medicaid enrollment card or eligibility letter.
FAQs
Can Medicaid work alongside other insurance?
What happens if someone is denied Medicaid?
Medicaid denials can happen for many reasons. Incomplete or incorrect applications, missing required documentation, or exceeding income limits are just a few. If there are errors on the application or significant life changes since denial—such as loss of income—applicants can reapply. This is called a Reversal, and the request must be submitted to an assigned caseworker. Individuals may also appeal a Medicaid denial, though this can be complicated. There is a 30- to 90-day window to request a Medicaid Fair Hearing where the individual can argue their eligibility with supporting evidence. This often requires an advocate or Medicaid attorney. Successful appeals will result in retroactive coverage from the date the original application was submitted.
Is there anything Medicaid doesn’t cover?
Medicaid is designed to cover essential health needs for qualifying individuals. While there are many additional and alternative treatments available, not all of these are covered under Medicaid, such as:
- Non-medically necessary dental procedures (cosmetic) and minor orthodontic treatments
- Elective cosmetic surgery
- Non-prescription drugs and health supplements
- Experimental treatments
- Elective abortions
- Home modification to accommodate disabilities
- Non-emergency medical transportation
- Homeopathic and alternative treatments
Medicaid maintains a dedicated network of healthcare providers, and healthcare services beyond that network may also not be covered unless Prior Authorization is given.
What is Medicaid Expansion?
Under the Affordable Care Act (ACA) certain U.S. states have extended Medicaid coverage to qualifying adults aged <65 years suffering from low income and financial hardship. To date, 41 states have adopted Medicaid expansion, excluding:
- Wyoming
- Kansas
- Texas
- Wisconsin
- Tennessee
- Mississippi
- Alabama
- Georgia
- South Carolina
- Florida
Ineligible residents of states that have not adopted Medicaid expansion should pursue alternative federal and state-level assistance and benefits programs.
What is Medicaid Share of Cost?
Medicaid Share of Cost (SOC) is the amount of money individuals and families must pay toward their medical expenses before their Medicaid policy will contribute, similar to a deductible. Also called “spend-down,” SOC is for individuals whose income exceeds Medicaid limits but who still have significant, unaffordable medical expenses. SOC amounts are determined by state Medicaid programs based on income and household size, and they can vary month to month.